Are you practicing balance?
You’ve worked so hard to get to where you are. You’ve studied and trained to do amazing things like save lives and change policies… yet you often don’t feel like you’re doing enough at work, or at home. Or for yourself.
Stop the overwhelm of trying to be all the things to all the people.
College. Grad school. Med school. Law school. Subspecialty training. Promotions. Making partner. It’s easy in our world to get caught on the hedonic treadmill of achievement… if you’re aware enough to look up, you just might realize you don’t know who you are anymore.
Let me help you find solutions for self-knowledge, self-care, and simplicity.
I got stuck on the treadmill and might still be there if I hadn’t had a major health scare to knock me down and into a journey of self-awareness and intentionality. Don’t make the mistakes I made; start working toward your own unique blend of work and life today!
Schedule a call
Read more about my self-knowledge journey and how I’ve come to practice medicine on my own terms.
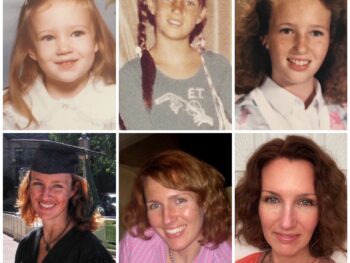
Who I am
I’m Dawn Baker. I’m a wife, a mother, a former engineer, and a board-certified anesthesiologist. I’m a lover of words and writing. I’m a keynote speaker, and I’m a lifestyle design coach for physicians and professionals.
I started my adult life as a vagabond rock climber and world traveler who loved to learn new things – which is what led me to a career in medicine. Only I lost myself on the way, as I got caught up in the treadmill of achievement. I forgot who I really was.
It took a cancer diagnosis, surgery, and recovery (and lots of coaching from various sources) to regain my balance, remembering my deeply-held values.
I’m now successfully practicing my balance. But my balance won’t look like your balance. Let me help you find yours.
Recent Blog Posts